Abstract
Background: Immune checkpoint inhibitors (ICIs) have been increasingly used in both solid and hematologic malignancies. In accordance with the mechanism of ICIs, they are associated with a spectrum of autoimmune toxicities termed immune-related adverse events (irAEs), including the poorly studied immune-related hematologic toxicity. Autoimmune destruction of hematopoietic stem cells is a common pathway for most cases of sporadic aplastic anemia (AA). However, few studies have investigated the incidence and outcomes of AA following ICI use.
Methods: Data was obtained from the TriNetX Research Database, a comprehensive network of protected patient data compiled from electronic health records, claims, and tumor registries. Specific ICIs studied include pembrolizumab, nivolumab, ipilimumab, durvalumab, and atezolizumab. Adult patients with newly diagnosed AA following treatment with ICIs were identified between 1/1/2015 and 1/1/2022. A diagnosis of AA was based on the ICD-10-CM codes D61.1 (Drug-induced aplastic anemia), D61.2 (Aplastic-anemia due to external agents), and D61.9 (Aplastic anemia, unspecified).
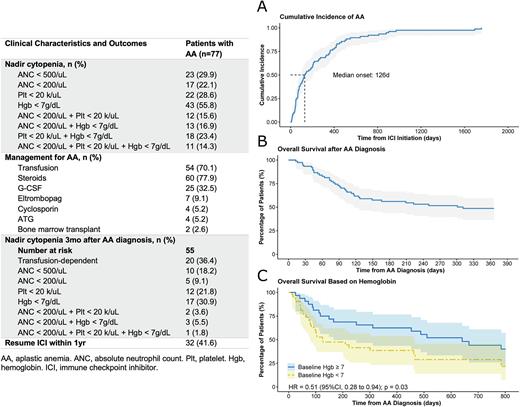
Results: During this study period, of the 52,203 patients treated with ICIs, 77 (0.15%) patients developed AA, in a median of 126 days after ICI initiation (Fig A). Of the 77 patients who developed AA, nivolumab was most used, followed by pembrolizumab and ipilimumab. For baseline nadir blood counts, 23 (29.9%) patients had an absolute neutrophil count (ANC) < 500/mL, 17 (22.1%) had an ANC < 200/mL, 22 (28.6%) had a platelet count < 20 k/mL, and 43 (55.8%) had a hemoglobin < 7g/dL; of note, 11 (14.3%) patients had severe pancytopenia (Table). In terms of treatment, 60 (77.9%) patients received glucocorticoids and 25 (32.5%) received G-CSF; only 7, 4, and 4 patients received eltrombopag, cyclosporin, and ATG, respectively. Of note, 2 patients underwent allogeneic hematopoietic stem cell transplantation. Three months after AA diagnosis, 20 (36.4%) remained transfusion dependent, while 5 (9.1%), 12 (21.8%), and 17 (30.9%) patients continued to have ANC < 200/mL, platelet count < 20 k/mL, and hemoglobin < 7g/dL, respectively; 1 patient remained to have severe pancytopenia (Table). Moreover, 37 deaths occurred within the first year, with a steep decline in overall survival (OS) in the first 120 days after AA diagnosis (Fig B). Patients with baseline nadir hemoglobin greater than 7g/dL had significantly better OS compared with those with nadir hemoglobin less than 7 g/dL (hazard ratio 0.51, 95% confidence interval 0.28 to 0.94; p=0.03, log-rank test; Fig C).
Conclusions: ICI-related AA is a rare event, with most cases occurring within the first 6 months following initiation of ICI. Glucocorticoids were the most used treatment. While most patients had improvement of cytopenia, a subset of patients were resistant to treatment and experienced prolonged cytopenia, resulting in a marked increase of mortality.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal